conditions
Peripheral Artery & Vascular Disease
The buildup of fatty deposits in your arteries doesn’t just affect your heart. It can also cause narrowing of the arteries in the rest of your body, leading to a condition called peripheral artery and vascular disease.
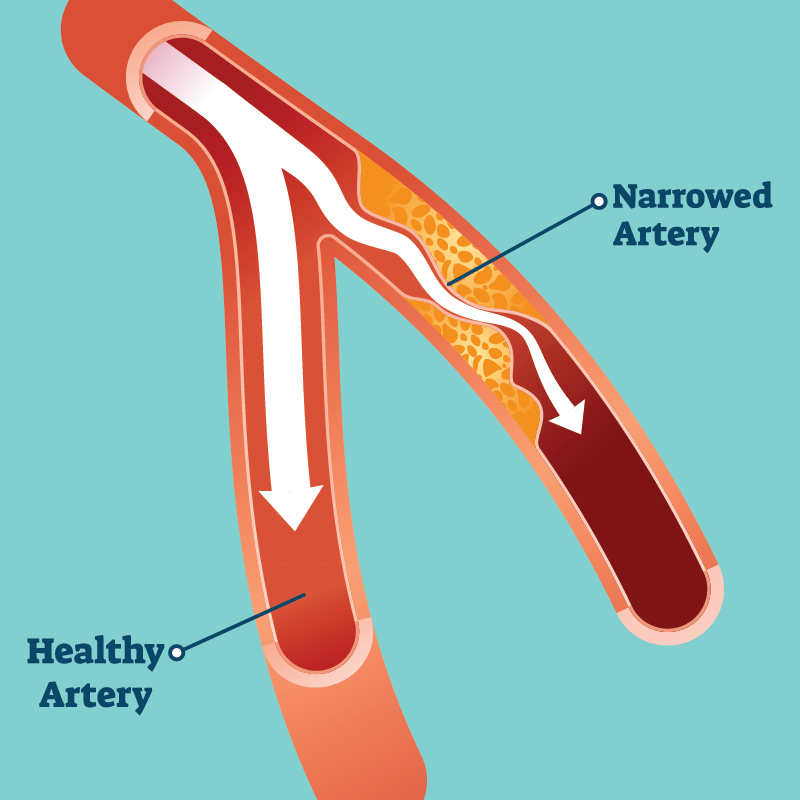
When fatty deposits called plaque build up on the walls of an artery, they gradually cause the blood vessel to become narrower. This buildup, called atherosclerosis, can occur in any artery in your body. When it occurs in the arteries of the heart, the condition is referred to as coronary artery disease. When it occurs in the limbs, it’s called peripheral artery and vascular disease, or PAD.
PAD reduces blood flow to the extremities, especially the legs. This condition does not always cause symptoms in its early stages, but PAD can be dangerous if left untreated.
Most people with PAD experience some pain in their legs when walking. This symptom is called claudication, and it tends to occur during physical activity and then subside after several minutes of rest. Calf pain is the most common symptom of PAD, but you might also notice numbness or weakness in one leg, a cold sensation in your leg or foot, a color change in the skin on your legs, or slower-than-usual toenail growth.
Additional symptoms of PAD can include shiny skin on the legs, hair loss or slower hair growth on the legs or ankles, and erectile dysfunction in men. Sores on your legs, feet, or toes that won’t heal may also be a sign of PAD. Without proper treatment, PAD may progress until you experience pain in your legs even when resting, a symptom called ischemic rest pain.
Because these symptoms often develop slowly, it’s important to be aware of the signs of PAD so you can seek medical care as early as possible. PAD symptoms mean that your arteries are becoming narrower, and if left untreated, this condition can lead to serious health emergencies.
Peripheral artery and vascular disease most often occur as a result of lifestyle factors or a pre-existing medical condition. Tobacco use and obesity significantly increase the likelihood of developing PAD. You’re also at higher risk of PAD if you have diabetes, hypertension, high cholesterol, or high levels of homocysteine (a protein that helps maintain muscle tissue). Being over the age of 50 is considered a risk factor. A family history of PAD may also play a role.
In rare cases, PAD may result from radiation exposure, limb injury, blood vessel inflammation, or unusual anatomy involving the muscles or ligaments.
In order to develop a treatment plan for your peripheral artery and vascular disease, your doctors first need to evaluate the severity of your atherosclerosis. This evaluation may involve a physical exam, ultrasound, blood tests, or use of the ankle-brachial index to compare the blood pressure in your ankle to that in your arm. In treating PAD, we focus on managing pain and reducing symptoms, but we also work to prevent your atherosclerosis from getting worse.
Medications that reduce blood pressure, control blood sugar, reduce clotting, or lower cholesterol can be helpful in managing PAD. Supervised exercise programs may also be beneficial. In some cases, surgery may be required to reduce claudication. Making recommended lifestyle changes and visiting your cardiologist regularly can help to manage or even prevent PAD.

